Credentialing Services
Atlantic Billing Solutions offers reliable and efficient Credentialing services for healthcare providers. Our experienced team handles the complex credentialing process, ensuring your practice is enrolled with insurance networks and compliant with industry regulations. Streamline your credentialing with our expert support.
Account Receivable Management Services (AR calling)
One of the most crucial elements in AR operations is coordination between AR callers and AR Analysts, because the analyst is responsible for monitoring an entire spectrum of outstanding debts owed to the medical facility, and the probability of repayment in a timely manner. The AR calling activities include coordinating with the billing team doctors office, Insurance companies, and patients.
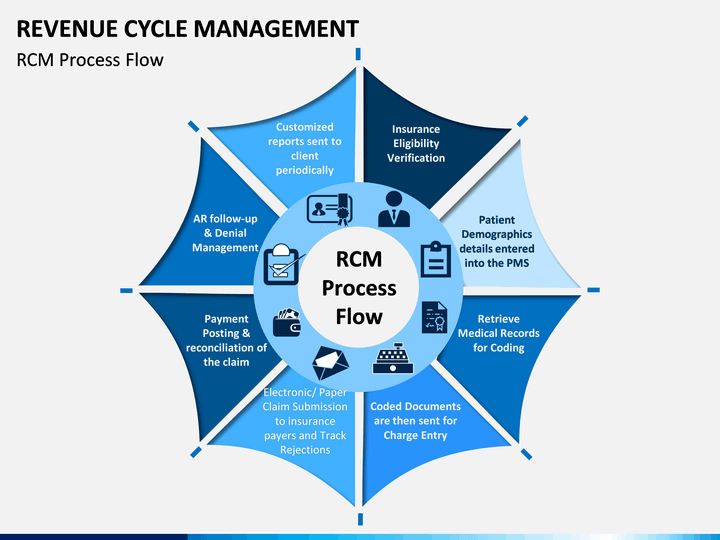
RCM Services
Optimize the many moving parts of your revenue cycle with BillingParadise’s podiatry revenue cycle management services. Our certified revenue cycle specialists will improve the compliance and performance of your podiatry RCM processes.
Coding Support Services
Atlantic Billing Solutions offers reliable and efficient Coding Support services for healthcare providers. Our team of certified coding experts ensures accurate and compliant medical coding, reducing claim denials and optimizing revenue. Elevate your practice with our specialized coding support.


Patient Eligibility & Verification Benefits
The rate of payment for the provider and patient dramatically improves if verification is accomplished ahead of time. Using our proprietary Real-Time Patient Eligibility Verification Tool the patient’s eligibility can be verified within minutes. The advance insurance coverage verification leverages practice to determine the total responsibility for the patient upfront.
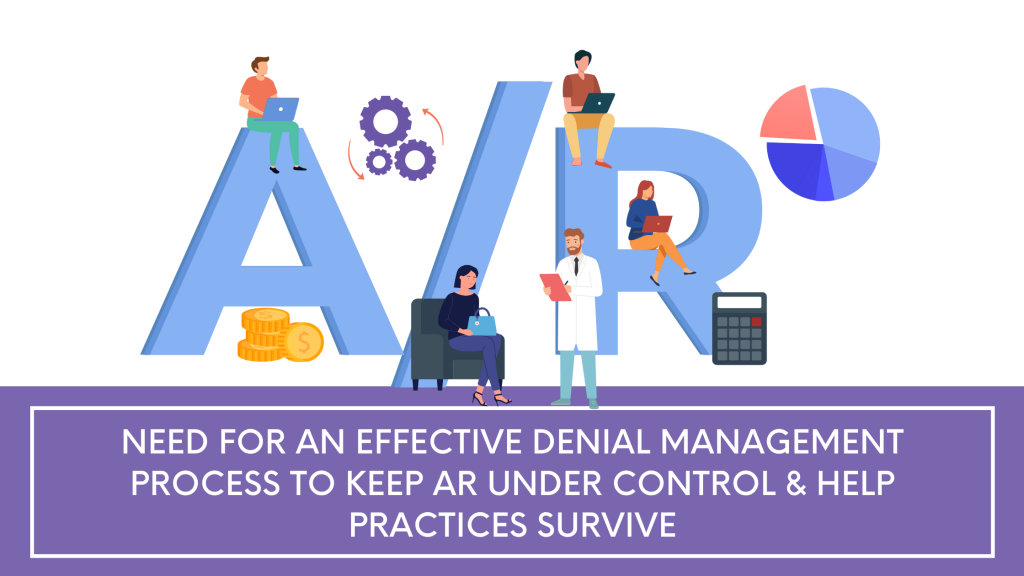
Denial Management
Denial is Management is a prolonged process needing professional supervision and a dedicated team. Medical practices lose valuable time processing denials, keeping them away from delivering quality patient care.
As a critical element of maintaining a healthy cash flow, our denial management team determines the causes of denials, and through a proven methodology using systematic best practices, we not only restore the cash flow of the organization, but also eliminate the risk of future denials.

Payment Posting
An efficient payment posting process helps a practice watch daily trends and determine areas of opportunity to increase revenue. The practice experiences greater growth when payment posting is done with efficacy. Billing issues are resolved quickly, secondary payers will be billed accurately, and statements to patients will be sent expeditiously.
